Introduction
The Accreditation Council on Graduation Medical Education’s (ACGME) Clinical Learning Environment Review (CLER) pathways provides a clear opportunity to connect Maintenance of Certification initiatives, hospital/system priorities for quality and safety, with graduate medical education. Through partnership with our GME-CLER leaders, we have identified opportunities for win-win initiatives that meet MOC, GME and system needs.
Objective
To elucidate the process steps associated with connecting GME and MOC using a patient safety/quality example.
Methods
Step #1: Start the Conversation Between Clinical, GME, and MOC /CPD Leaders
MOC leaders meet with GME and ask to review CLER related documents and site visit reports.
Step #2: Identify Shared Pain/Performance Improvement Needs/Targets
Joint Commission and the ACGME CLER Patient Safety (PS) Pathway 1 highlight the importance of incident reporting. Per CLER, reporting is “an important mechanism to identify patient safety vulnerabilities,” yet physician reporting is low relative to other professions = A cross cutting performance improvement target.
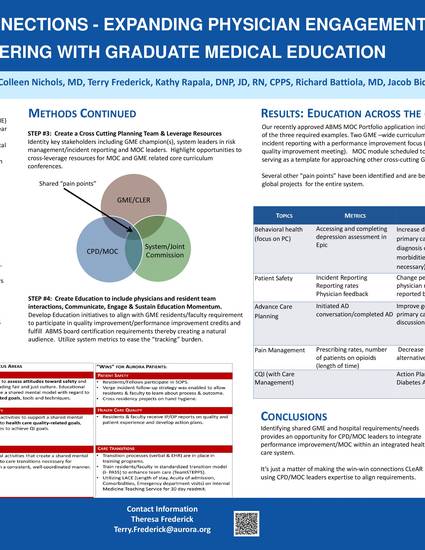
Step #3: Create a Cross Cutting Planning Team & Leverage Resources
Identity key stakeholders including GME champion(s), system leaders in risk management/incident reporting and MOC leaders. Highlight opportunities to cross-leverage resources for MOC and GME related core curriculum conferences.
Step #4: Create MOC, Communicate & Engage
Develop MOC initiative to align with GME residents/faculty requirement to participate in quality improvement /performance improvement processes thereby creating a natural audience. Utilize system metrics to ease the “tracking” burden.
Results
Our recently approved ABMS MOC Portfolio application included incident reporting as one of the three required examples. Two GME –wide curriculum sessions have focused on incident reporting with a performance improvement focus (abstract accepted at national quality improvement meeting). MOC module scheduled to go live spring 2016. Approach is serving as a template for approaching other cross-cutting GME/Hospital/System needs.
Conclusions
Identifying shared GME and hospital requirements/needs provides an opportunity for CPD/MOC leaders to integrate performance improvement/MOC within an integrated health care system. It’s just a matter of making the win-win connections CLeAR and using CPD/MOC leaders expertise to align requirements.
Ouweneel K, Nichols CM, Simpson D, Rapala K, Battiola R, Bidwell J, Frederick T, Su H. Making CLEaR Connections – Expanding Physician Engagement in QI by Partnering with Graduate Medical Education. [Selected for the Portfolio Program Sponsor Poster Challenge] American Board of Medical Specialties Quality Improvement Forum 2016. Rosemount, IL. May 11, 2016

Continuing Professional Development
Aurora Health Care
Internal Medicine Residency