Background: Substance use disorder (SUD) is diagnosed in 10% of the U.S. population across a lifetime. Although around 10% of individuals with SUD go into long-term remission each year, the disease is considered chronic and is punctuated by many periods of abstinence, relapse, and eventual long-term remission. Nevertheless, only 35%–50% of individuals with SUD experience long-term remission within 17 years of diagnosis. To account for disease chronicity and varying levels of need over time, several treatment programs exist, each tailored to an individual’s current acuity and needs. These treatments include inpatient, residential, partial hospitalization program (PHP), intensive outpatient program, and outpatient treatment. Patients are assessed and referred for a specific level of treatment, and individual outcomes are superior if patients enter and complete the recommended program. However, many patients choose to reduce their lengths of stay, discharge against medical advice, or enter programs mismatched with their current acuity.
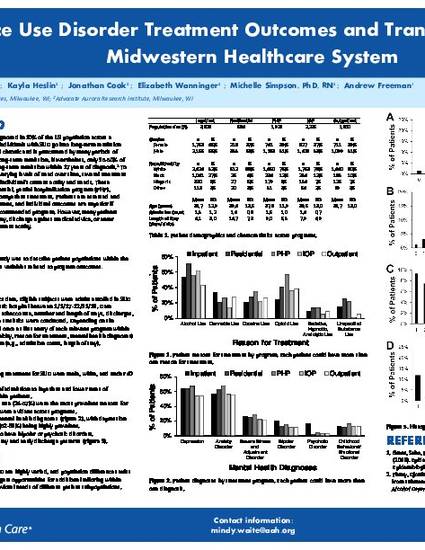
Purpose: This retrospective study describes patient populations within the 5 unique SUD programs as well as variables related to program completion and length of stay.
Methods: Medical records were used to collect data. Eligible subjects were adults enrolled in SUD treatment at a midwestern psychiatric hospital between January 1, 2017, and November 20, 2019. Data included demographics, diagnoses, tobacco use, number and length of stays, referrals, discharge against medical advice, and program type. Basic descriptive statistics were conducted.
Results: Of the total population (N=4990), the majority of patients receiving treatment for SUD were male (59.9%), current smokers (61.8%), and had a mean age of 39.9 years. Further, many patients had concurrent mental health diagnoses; depression and/or anxiety disorders were prevalent in 53%–57% of patients. Within the context of substance use, patients were most likely to have been diagnosed with alcohol use disorder, opioid use disorder, cocaine use disorder, and cannabis use disorder. Similarly, patients were most likely to receive treatment for alcohol use, cannabis use, opioid use, and cocaine use. Co-occurring diagnoses were extremely common, and patients in PHP programming had the greatest number of diagnoses.
Conclusion: Patients receiving treatment for substance use disorder are highly varied, and population differences exist among programs. These data suggest opportunities for tailoring programs to meet the current and long-term needs of patients.
Waite MR, Heslin K, Cook J, Wanninger E, Simpson M, Freeman A. Substance use disorder treatment outcomes and transitions at a large midwestern healthcare system. Poster presented at: Aurora Scientific Day; May 20, 2020; virtual webinar hosted in Milwaukee, WI.

Aurora Behavioral Health Services
Advocate Aurora Research Institute