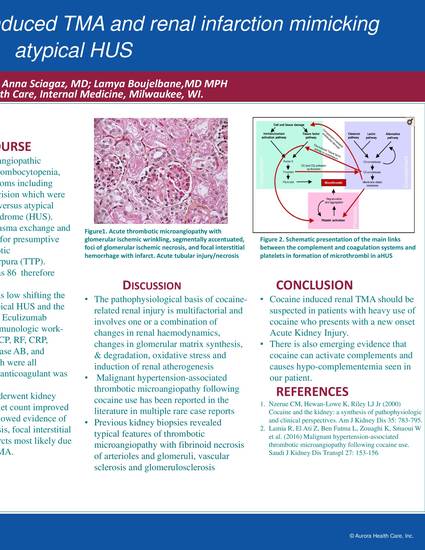
Introduction: Cocaine use has known association with fatal medical complications, including myocardial ischemia, cerebrovascular accident, and kidney injury secondary to ischemia, rhabdomyolisis, and malignant hypertension. However, cocaine induced Thrombotic microangiopathy (TMA) and renal infarction is a rare entity that has not been described in the literature except in few case reports. Case Presentation: A 24-year-old female with a past medical history of alcohol and cocaine abuse was admitted with alcoholic induced acute pancreatitis and acute anuric renal injury. She developed microangiopathic hemolytic anemia, thrombocytopenia, and neurologic symptoms including headache and blurry vision which were concerning for TMA versus atypical hemolytic uremic syndrome (HUS). Her labs showed creatinine 7 mg/dL with a baseline of 0.7–0.9 mg/Dl, thrombocytopenia (PLT 40), schistocytes on peripheral smear, a drop in hemoglobin (from 9 to 5.6 g/Dl), with elevated total bilirubin 3.2 g/dL and LDH 3400. She was started on plasma exchange and IV mehtylprednisone for presumptive diagnosis of Thrombotic thrombocytopenic purpura (TTP). ADAMTS13 level was 86 which is normal, therefore TTP was ruled out. Complement level was low shifting the diagnosis toward atypical HUS and the patient was started on Eculizumab. Further workup include immunologic work-up including ANA, CCP, RF, CRP, C3/ C4, myeloperoxidase AB, and proteinase-3 AB which were all unremarkable. Lupus anticoagulant was positive. Finally the patient underwent kidney biopsy once her platelet count improved and the final report showed evidence of ATN, ischemic necrosis, focal interstitial hemorrhage, and infarcts most likely due to cocaine induced TMA. Conclusion: Cocaine induced renal TMA should be suspected in patients with heavy use of cocaine who presents with a new onset Acute Kidney Injury. There is also emerging evidence that cocaine can activate complements and causes hypo-complementemia seen in our patient.
Odeh K, Scigacz A, Boujelbane L. Unique case of cocaine induced TMA and renal infarction mimicking atypical HUS. American College of Physicians - 2018 Wisconsin Chapter Annual Scientific Mtg. Storyboard. September 7-8, 2018. Wisconsin Dells, WI.

Aurora St. Luke's Medical Center
Aurora Sinai Medical Center