- School of Anesthesia
Background With 47,600 opioid overdose related deaths in the U.S. in 2017, the opioid crisis is of national concern.1 Cesarean delivery is the most common surgery worldwide, with over 1.2 million in the U.S. in 2018 alone.2,3 As cesarean delivery is a highly prevalent surgery it has a large capacity to influence the opioid epidemic. Literature is showing that Enhanced Recovery after Surgery (ERAS) and multimodal analgesia are effective means of managing postoperative pain while minimizing opioid use.4,5,6,7,8 This project aims to help discover if introduction of ERAS, and more specifically it’s multimodal analgesia aspect, has helped decrease oral morphine milligram equivalent (MME) consumption of opioids following cesarean delivery.
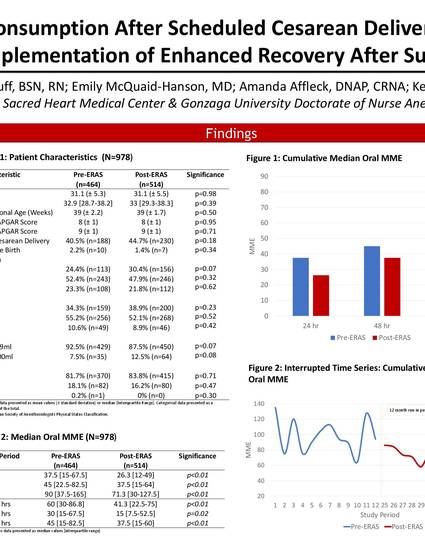
Methods • Design: Retrospective Observational Cohort Study • Human Subjects Protection: Data fully de-identified and stored only in a secure REDCap database; patient care was not altered • Inclusion Criteria: Adult women undergoing scheduled cesarean delivery at Providence Sacred Heart Medical Center, Spokane, WA • Exclusion Criteria: Urgent/emergent cesarean delivery, use of an intravenous opioid patient-controlled analgesia (PCA) device • Measured Outcome: Cumulative 72-hr oral MME consumption following cesarean delivery • Baseline Comparability Demographics: Age, ASA, BMI, gravida/parity, weeks gestation, prior cesarean delivery, multiple birth, estimated blood loss, etc. (table 1) • Statistical Analysis: • A Priori Power Analysis: n=670 (n=335 per group) participants for adequate power (α=0.5, β=0.2) • Bivariate Analysis: Independent Samples T-Test (symmetrical data) and Mann Whitney U Test (skewed data) • Multivariate Analysis: An interrupted time series was conducted for comparison of oral median MME over time • Split File Analysis conduced to confirm accuracy of findings
Discussion The implementation of ERAS and use of multimodal analgesia led to a sustained MME decrease among women utilizing opioids post scheduled cesarean delivery. The pre-implementation group (n=464) utilized a median of 90 [IQR 37.5-165] oral MME while the post-implementation group (n=514) used 71.3 [IQR 30-127.5] median oral MME (p<0.01). This was a difference of 18.7 oral MME, or a 21% reduction. The use of multimodal analgesia following scheduled cesarean delivery is an effective means of managing postoperative pain while also reducing the need for opioids.
Available at: http://works.bepress.com/kenn-daratha/44/
