Introduction/Background
Success in today’s complex and evolving health care settings requires that leaders be able to guide problem finding and solving teams. Lack of leadership skills – particularly in the areas of systems-based practice, professionalism, and communication – has been linked to patient harm. The need for leadership training is recognized across health care as programs are offered through graduate medical education (GME) offices and residency programs, hospitals, and health care systems. GME sponsored leadership programs may cross medical specialties but typically they do not professions. In contrast, leadership programs at the hospital/system level are often interprofessional in nature (e.g., physicians, RNs, quality directors, financial leaders, pharmacists, allied health professions) mirroring the multi-disciplinary nature of health care teams but do not include residents. While integrating residents into these established interprofessional leadership development programs would be a win-win for GME and our sponsoring organizations a review of the GME-related leadership literature yielded no models for this approach.
Hypothesis/Aim Statement
To integrate residents into an established interprofessional hospital leadership program.
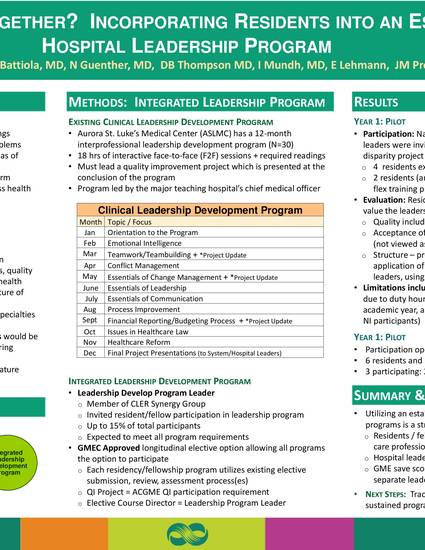
Methods
Aurora St. Luke’s Medical Center (ASLMC) has a 12-month interprofessional leadership development program with topics common to resident focused leadership programs: teamwork/teambuilding, conflict and change management, leadership and communication essentials, process improvement and finance/budgeting. ASLMC’s program format includes 18 hours of interactive face-to-face (F2F) sessions, required readings, and leadership of a quality improvement project presented at the conclusion of the program. The hospital’s chief medical officer leads the program and as a member of the CLER synergy leadership group, exceeded an invitation to GME to include residents.
Results
National Initiative (NI) resident leaders were invited to participate during the pilot year with their NI disparity project meeting the program’s requirement. Four residents expressed interest with two residents (and their program director) able to flex training program schedules and met program requirements as a longitudinal elective. Residents are periodically debriefed about their participation reporting that they strongly value the leadership program’s quality, the opportunity to participate as a physician (not viewed as resident) in an interprofessional program, and the ability to apply key concepts/principles from the program to NI work. Limitations include inability to attend F2F sessions due to duty hours, synching calendar year with academic year, and limited project time (true for all NI participants independent of leadership program participation).
Conclusions
Utilizing an established hospital based interprofessional leadership programs is a strong ROI: residents engage with other health care professionals learning as peers gaining valued skills to support NI project, hospital leaders gain from residents’ perspectives, GME’s saves costs associated with sponsoring a separate leadership program.
Su H, Abel I, Battiola R, Guenther N, Thompson D, Mundh I, Lehmann E, Simpson D. Separate or Together? Incorporating Residents into an Established Hospital Leadership Program. AIAMC Annual Meeting. March 30– April 1, 2017. Amelia Island, FL.

Aurora St. Lukes Medical Center
Aurora Sinai Medical Center