Discussing what matters most: designing a medical student curriculum for end-of-life care
Natanya S. Russek, Karrie Lu, Kjersti Knox, Timothy Jessick
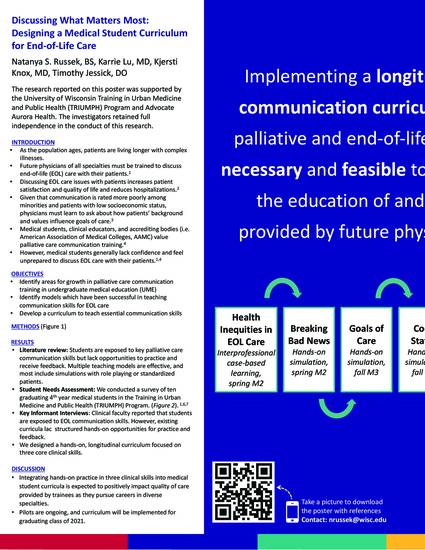
Background: As the population ages, patients are living longer with complex illnesses. While physicians of all specialties are expected to provide patient-centered end-of-life care, studies demonstrate that medical students lack comfort discussing these topics with patients. Our aims were to identify gaps in medical student education and to design and implement a hands-on, longitudinal curriculum to teach essential skills for providing compassionate and skillful care to patients nearing the end of life.
Methods: We followed the six-step approach for medical curriculum development: problem identification, needs assessment, goal-setting, identifying educational strategies, implementation, and evaluation development. We reviewed national and local curricula and surveyed graduating medical students. Goals, objectives, and curriculum design were developed with input from student and faculty interviews. Qualitative and quantitative evaluation is ongoing.
Results: Literature review revealed that students are exposed to goals of care, breaking bad news, and code status discussions. However, students lack opportunities to practice and receive feedback on these skills. Ten students training as a cohort in a longitudinal clinical and urban medicine program were surveyed in a needs assessment prior to graduation; all reported exposure to goals of care conversations and 10% reported confidence. Similarly, 100% reported exposure to breaking bad news but only 20% reported confidence. The curriculum includes multiple hands-on teaching sessions where students practice breaking bad news and goals of care conversations. Peers and physician facilitators observe and provide active feedback during mock patient interviews. The initial iteration of the curriculum has been received with positive feedback.
Conclusions: Implementing a longitudinal curriculum in palliative and end-of-life care is necessary and feasible to improve education of future physicians. Students are expressing increased confidence after a few sessions, and training is ongoing. Future curriculum evaluation will include comparison of experience and confidence in key clinical skills before and after exposure to this novel curriculum. Integrating hands-on practice in these critical skills into medical student curricula will impact the quality of care provided by trainees as they pursue careers in diverse specialties.
Natanya S. Russek, Karrie Lu, Kjersti Knox, Timothy Jessick. Discussing what matters most: designing a medical student curriculum for end-of-life care. J American Geriatrics Society. 2019:67(S1);S321

Aurora St Luke's Medical Center