Background: A recent study of 244 subjects looked into clinical outcome of colonoscopy based on the physician’s awareness of the positive stool DNA test result. The study compared unblinded unmonitored colonoscopy with blinded monitored colonoscopy.
Purpose: We present a larger real-life study on the impact of physician awareness of a positive stool DNA test on colonoscopy results.
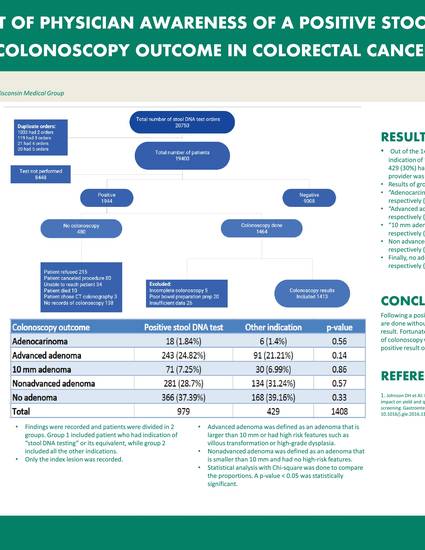
Methods: Chart review of 1413 patients who had a positive stool DNA followed by documented subsequent colonoscopy was done. Attention was paid to the indication of the procedure in the colonoscopy report. A total of 5 patients were excluded; 3 of these had unknown indication and 2 a finding of “other carcinoma.” Findings were recorded and patients were divided into two groups. Group 1 included patients who had indication of “stool DNA testing” or its equivalent, while group 2 included all the other indications. Only the index lesion was recorded. Advanced adenoma was defined as an adenoma larger than 10 mm or that had high-risk features such as villous transformation or high-grade dysplasia. Nonadvanced adenoma was defined as an adenoma smaller than 10 mm with no high-risk features. Statistical analysis with chi-squared was done to compare the proportions. A P-value less than 0.05 was considered statistically significant.
Results: Of the 1408 patients, 979 (70%) had an indication of “stool DNA testing” or its equivalent, while 429 (30%) had another indication (to which we assumed the provider was not aware of the positive stool DNA testing). Results of group 1 and group 2 were as follows: Adenocarcinoma was found in 1.8% vs 1.4%, respectively (P=0.56); advanced adenoma was found in 24.8% vs 21.2%, respectively (P=0.14); >10-mm adenoma was found in 7.25% vs 6.99%, respectively (P=0.86); and nonadvanced adenoma was found in 28.7% vs 31.2%, respectively (P=0.57). Finally, no adenomas were found in 37.4% vs 39.2%, respectively (P=0.33).
Conclusion: Following a positive stool DNA test, 1 out of 3 colonoscopies are done without the physician’s awareness of the positive result. Fortunately, there was no difference in the outcome of colonoscopy whether the physician was aware of the positive result or not.
Fahed J, Affi A. Real-life impact of physician awareness of a positive stool DNA test on subsequent colonoscopy outcome in colorectal cancer screening. Poster presented at: Aurora Scientific Day; May 22, 2019; Milwaukee, WI.

Department of Gastroenterology, Aurora Health Care