Presentation
ABSTRACT NUMBER: 2872 Risk of 30-day Readmission and Adverse Events After Primary Hip or Knee Arthroplasty: A Comparison of Patients with Rheumatoid Arthritis versus Osteoarthritis Using the Nationwide Readmission Database
2019 ACR/ARP Annual Meeting
(2019)
Abstract
Background/Purpose: To assess the risk of 30-day readmission, mortality, and adverse events among adults with Rheumatoid Arthritis as compared to Osteoarthritis after primary hip or knee arthroplasty.
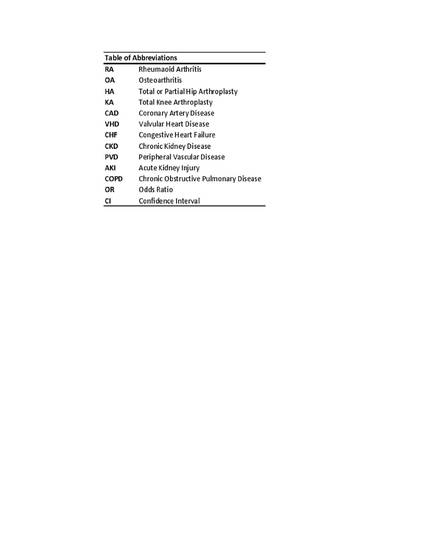
Methods: We identified index hospitalizations with a principal procedure of primary HA or KA using a nationally representative U.S. sample, the Nationwide Readmission Database (2010-2013). Excluded were persons aged < 18 years or who did not survive the index hospitalization. The principal procedure and diagnoses were identified using ICD-9 codes. Using survey logistic regression, we calculated the unadjusted and adjusted risk of 30-day readmission, all-cause mortality, and composite adverse events which included infections, cardiovascular events, venous thromboembolic events, mechanical complications, and AKI, after adjusting for age, sex, and major comorbidities.
Results: There were 1,977,214 index hospitalizations of which 10,802 were in persons with RA and 1,966,413 in persons with OA. Persons with RA were older (66.9 vs. 65.6; P< 0.01), more likely to be women (80.7% vs. 59.5%; P< 0.01), and to have existing comorbid conditions of CAD (10.0% vs. 8.0%;P< 0.01), chronic CHF (2.4% vs. 0.6%;P< 0.01 ), CKD (6.6% vs. 3.8%; P< 0.01), cancer (1.6% vs. 0.9%; P< 0.01), PVD (3.1% vs. 1.4%; P< 0.01), and COPD (20.8% vs. 14.0%; P< 0.01). There were 68,897 (3.5%) 30-day readmissions. The readmission rate was higher among persons with RA compared to OA (7.1% vs. 3.5%; P< 0.001). Stratified readmission rates for RA versus OA were (9.3% vs. 3.4%; P< 0.001) and (4.2% vs. 3.5%; P=0.18) in HA and KA, respectively. The adjusted OR for readmission was 2.06 [ 95% CI: 1.75,2.42], all-cause mortality 9.87 [95% CI:5.02,19.41], and composite event 2.29 [95% CI:1.81,2.89]. In analyses stratified by procedure type, the adjusted OR post-HA for readmission was 2.35 [ 95% CI: 1.94,2.83], all-cause mortality 6.16 [95% CI:2.96,12.82], and composite event 2.32 [95% CI:1.79,2.99] while post-KA the risk of readmission was 1.36 [ 95% CI: 1.02,1.80], all-cause mortality 13.81 [95% CI:3.35,56.90], and 1.78 for composite event [95% CI:1.14,2.78]. The overall adjusted risk for mechanical complications [OR:4.38; 95% CI:2.56,7.47], all-type infections [OR:2.23; 95% CI:1.71,2.92], and AKI [OR:3.78; 95% CI:1.41,10.13] was higher in RA while the risk for CVD [OR:1.73; 95% CI:0.77,3.87], DVT/PE [OR:0.95; 95% CI:0.45,2.02], or surgical site infections [OR:1.51; 95% CI:0.98,2.31] did not differ relative to OA. In stratified analyses, the risk for AKI and all-type infections was higher among persons RA in both procedure types while the risk for mechanical complications was only significant in HA [OR:1.99; 95% CI:1.14,3.47].
Conclusion: After primary joint arthroplasty, the 30-day rehospitalization, all-cause mortality, and composite events were more likely among persons with RA relative to OA, even after accounting for demographics and major co-morbidities. All-type infections and acute kidney injury were more likely among person with RA after both hip and knee arthroplasty, while mechanical complication was significantly higher in persons with RA as compared to OA only after hip arthroplasty.
Disciplines
Publication Date
November 13, 2019
Citation Information
Anthony A. Donato, Ali Yazdanyar, Kathleen McElwee, Mary C Wasko, et al.. "ABSTRACT NUMBER: 2872 Risk of 30-day Readmission and Adverse Events After Primary Hip or Knee Arthroplasty: A Comparison of Patients with Rheumatoid Arthritis versus Osteoarthritis Using the Nationwide Readmission Database" 2019 ACR/ARP Annual Meeting (2019) Available at: http://works.bepress.com/anthony-donato/34/
