Outcomes of Patients on Extracorporeal Membrane Oxygenation (ECMO) for Periods of Time Without Anticoagulation at LVHN in the Past 3 Years
Bryan Auvil, Rosalie Mattiola, Rita Pechulis, MD, James Wu, MD
Department of Surgery, Division of Cardiothoracic Surgery
Lehigh Valley Health Network, Allentown, PA
Abstract
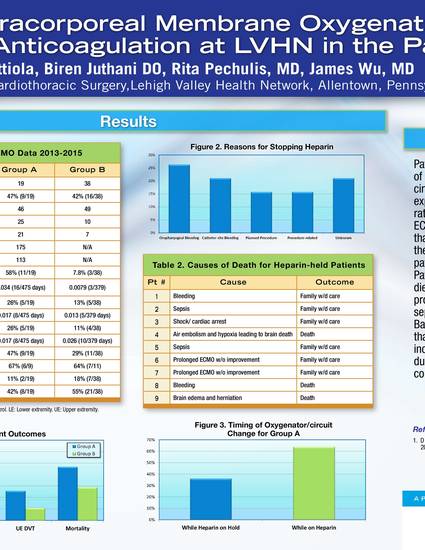
Extracorporeal membrane oxygenation (ECMO) is an aggressive life support technique that utilizes extracorporeal circuits and oxygenators to support severe lung injury such as acute respiratory distress syndrome (ARDS), as well as severe cardiac disorders like cardiogenic shock and cardiac arrest. Veno-Venous (VV) ECMO is primarily used in respiratory distress. Clots can form within the oxygenator or circuit, which can develop embolic complications or flow problems. To prevent this, patients are anticoagulated, usually with heparin. However patients can develop bleeding complications, and therefore must have their AC discontinued. A retrospective chart review was done on 57 VV ECMO patients, out of which 19 had their heparin held for at least one period of 24 hours or longer. Temporarily non-heparinized patients required far more oxygenator and circuit replacements than control (58% compared to 8% of patients), had more DVTs (37% compared to 21%), and had a higher mortality rate (47% compared to 29%), however the rates of DVT per day on ECMO were very similar. Patients in the non-heparinized cohort died when the families withdrew care because of prolonged ECMO without improvement, worsening sepsis, and/or severe bleeding complications. Based on these findings there is no direct evidence that temporarily discontinuing AC resulted in increased patient mortality. This was more likely due to increased severity of illness and bleeding complications, evidenced by the increased time on ECMO.
Keywords
Extracorporeal membrane oxygenation, ECMO, Veno-venous ECMO, VV ECMO, heparin, anticoagulation, DVT, thrombosis, thrombotic complication
Introduction
Extracorporeal membrane oxygenation (ECMO), also known as extracorporeal life support (ECLS) is a very aggressive technique that utilizes extracorporeal circuits and oxygenators to support severe lung injury such as acute respiratory distress syndrome (ARDS), as well as cardiac support for cardiogenic shock and cardiac arrest. There are two major categories of ECMO: Veno-Venous ECMO is primarily used in respiratory distress, using a right internal jugular vein access; and Veno-Arterial ECMO is primarily used for cardiac or cardiopulmonary support, using femoral vein and artery access1. Extra Corporeal Life Support (ECLS) is sometimes used synonymously.
Blood that comes into contact with foreign surfaces tends to coagulate. Clots that form within the oxygenator and extracorporeal tubing can be pushed into the patient and ultimately cause a thrombus, or in severe cases, a stroke. Therefore, as part of the protocol for extracorporeal circuits, patients undergo anticoagulation (AC) therapy and are uniformly heparinized with a partial thromboplastin time (PTT) in the range of 50-70 seconds, and an activated clotting time (ACT) of 180-200 sec2.
Some of these severely ill patients can develop bleeding complications involving the oral pharyngeal cavity, abdominal cavity, thoracic cavity, and cannulation sites. In these cases, because of ongoing bleeding and exploratory surgery, AC needs to be stopped, sometimes for prolonged periods of time. Other patients are coagulopathic due to their illness, and therefore don’t receive therapeutic AC.
Major bleeding is defined as clinically overt bleeding associated with a hemoglobin (Hgb) fall of at least 2 g/dl in a 24 hour period, greater than 20 ml/kg over a 24 hour period, or a transfusion requirement of one or more 10 ml/kg packed red blood cell (PRBC) transfusions over that same time period. In addition, bleeding that is retroperitoneal, pulmonary or involves the central nervous system, or bleeding that requires surgical intervention would also be considered major bleeding. Minor bleeding would be considered less than 20 ml/kg/day and require transfusion of one 10 ml/kg PRBC transfusion, or less. This is significant, because hemorrhagic complications and the requirement for greater red blood cell transfusion volumes are associated with increased mortality in both cardiac and non-cardiac ECLS2.
The ultimate goal of this project was to review the safety and outcome of patients on ECMO in whom therapeutic anticoagulation is held secondary to bleeding complications, as there is no significant body of literature regarding this topic.
Methods
This retrospective study involved 57 VV ECMO patients (47% male, average age: 48) selected from the hospital database. Patients were sorted based off of the following inclusion criteria: (1) Patient had to have been on VV ECMO at LVHN since 2013, and (2) Patient had to be at least 18 years old. Of the 57 patients, 19 had their heparin held for at least one period of 24 hours or longer. All patients’ electronic medical records (EHMR) were examined to determine incidence of upper extremity (UE) and lower extremity (LE) deep vein thrombosis (DVT), patient mortality, and possible link between thrombotic complications and patient outcomes. Thrombotic complications include stroke, ischemic limb, kidney and liver injury, and surgical procedures for bleeding from body cavities and insertion sites. Records were also examined to determine if/how many oxygenator or circuit changes were necessary. For patients whose heparin was held, the source of bleeding was determined.
Incidence of DVT, as well as need for oxygenator/circuit changes were calculated both as a percentage of the population, and as a rate of total events per total days on ECMO for that group. This was done in an attempt to normalize the data to account for the large difference between groups in average time spent on ECMO.
Results
The 19 patients whose heparin was held for a period of at least 24 hours (non-heparinized patients) spent an average of 25 days on ECMO, with an average AC hold time of 175 hours, while the 38 control patients spent an average of 10 days on ECMO (Table 1). The non-heparinized group was 47% male, with an average age of 46, and the control group was 42% male with an average age of 49 (Table 1).
58% of non-heparinized patients required oxygenator or circuit changes, at a rate of 0.034 changes per total day on ECMO (16 changes/475 days), while only 7.8% of control patients required changes, at a rate of 0.0079 (3 changes/379 days) (Table 1). 26% of non-heparinized patients and 13% of control patients experienced a LE DVT, but the rates were more similar at 0.017 (8 DVTs/475 days) and 0.013 (5 DVTs/379 days), respectively (Table 1). This trend continued with UE DVTs; although 26% of non-heparinized patients experienced an UE DVT compared to 11% of control patients, non-heparinized patients’ rate of 0.017 (8 DVTs/475 days) was actually lower than control patients’ rate of 0.026 (10 DVTs/379 days) (Table 1).
The mortality rate for non-heparinized patients was 47% (9/19), with 6 out of 9 patients’ families deciding to withdraw care. The mortality rate for control patients was 29% (11/38), with 7 out of 11 patients’ families deciding to withdraw care (Table 1). 11% (2/19) of non-heparinized patients were discharged home and 42% (8/19) were discharged to rehab facilities, while 18% (7/38) of control patients were discharged home and 55% (21/38) were discharged to rehab facilities (Table 1).
Reasons for discontinuing heparin or other AC included hemoptysis (7/19) and oropharyngeal (5/19), tracheotomy site (6/19), and cannula site (6/19) bleeding. VV ECMO patient etiology included H1N1 (28%), pneumonia (16%), aspiration (14%), Legionella (9%), post-operative complications (7%), MI and cardiac arrest (5%), and other illnesses (9%). Etiology was unknown for 12% of patients (Figure 3).
Non-heparinized patients died due to severe bleeding, sepsis, hypoxia-related brain death, and family withdrawing care due to prolonged ECMO treatment without improvement (Table 3).
Conclusions
Patients whose heparin was held for period(s) of at least 24 hours required oxygenator and circuit changes much more frequently. They also experienced more DVTs and had a higher mortality rate; however, their overall rate of DVTs per day on ECMO is similar that of the control group, indicating that the increased incidence of DVT is likely due to the significantly longer average amount of time those patients spent on ECMO relative to control patients. Patients in the non-heparinized cohort mostly died when the families withdrew care because of prolonged ECMO without improvement, worsening sepsis, and/or severe bleeding complications. There were no obvious systemic thrombotic complications. Based on these findings there is no direct evidence that temporarily discontinuing AC resulted in increased patient mortality. This was more likely due to increased severity of illness and bleeding complications, requiring more time on ECMO.
The study has quite a few limitations. It cannot necessarily be broadly applied due to the small sample size of only 57 total patients over three years, with an experimental group of only 19 patients. Furthermore, only statistics from a single hospital system were examined. However, the findings indicate that at least in this patient cohort, there was no obvious link between withholding anticoagulation therapy while on ECMO and increased patient mortality. This suggests that in contrast to standard ECMO protocol, it might be reasonable to withhold heparin from ECMO patients - at least temporarily - in the case of moderate to severe bleeding2. Further study is indicated to determine whether the results of this study are generalizable to a wider patient population, and whether discontinuing AC therapy in ECMO patients does in fact affect patient mortality.
Acknowledgements
James Wu, MD, Rita Pechulis, MD, Hope Kincaid, MPH, CPH, Jane Scott, Hubert Huang, Ph. D., Jordan Williams, Amanda Broderick, Alex Maryshina, Joseph Napolitano, Ph.D.
References
- D Brodie, M Bacchetta. Extracorporeal Membrane Oxygenation for ARDS in Adults. N Engl J Med 2011;365:1905-14.
- ELSO Anticoagulation Guideline 2014
Table 1: LVHN VV ECMO data 2013-2015
Table 2: Reasons for discontinuing heparin
Figure 1: Etiology of LVHN VV ECMO patients 2013-2015
Table 3: Causes of death for heparin-held patients
Figure 2: Patient complications and outcomes as percentage of total group
Figure 3: Rate of patient complications (total # of events per total days on ECM
Second Place - Best Overall Presentation
Second Place - Best Research Project
Second Place - Best Presentation
Auvil, B., Mattiola, R., Pechulis, R., Wu, J. (2015, July 31). Outcomes of Patients on Extracorporeal Membrane Oxygenation (ECMO) for Periods of Time Without Anticoagulation at LVHN in the Past 3 Years. Poster presented at LVHN Research Scholar Program Poster Session, Lehigh Valley Health Network, Allentown, PA.
Juthani, B. (2015, September 18). Outcomes of Patients on Extracorporeal Membrane Oxygenation (ECMO) for Periods of Time Without Anticoagulation at LVHN in the Past 3 Years. Poster presented at the 26th Annual Extracorporeal Life Support Organization Conference, Atlanta, GA.
Copyright © Lehigh Valley Health Network