Introduction/Background
Hypertension (HTN) is more prevalent in African Americans (51.7%) than white individuals (43.6%). African Americans are more likely to suffer adverse HTN consequences including cardiovascular disease and death. Among young African Americans (18-44 yo), 30% have HTN. This increased prevalence is attributable to many factors, including structural racism, distrust of the health care system, and access to care. In an urban primary care residency clinic, a disparity was noted in HTN control between young African American patients and young white patients.
Hypothesis/Aim Statement
Identity interventions associated with improved HTN control in urban, vulnerable, young (18-50 yo) African American patients in a primary care residency program.
Methods
In collaboration with a medical librarian, a literature search was conducted to identify interventions applicable to vulnerable urban African American populations. A spreadsheet was created for coding by publication year, article type, population studied, intervention, results, and barriers.
To identity what interventions might be most applicable to this population, we conducted a series of brief, structured phone interviews with open-ended and Likert scale items. Questions focused on the long-term effects of HTN, barriers to HTN control, and interest in working with a primary care physician to address their HTN including use of home blood pressure monitoring (HBPM). African American patients between 18-50 years whose blood pressure was not currently well-controlled were identified by the second author and vetted with clinic staff to determine responsiveness to discussing their care with a medical student. A random sample of those patients were then selected for interviews with replacement following 3 unsuccessful contact attempts for this quality improvement effort.
Results
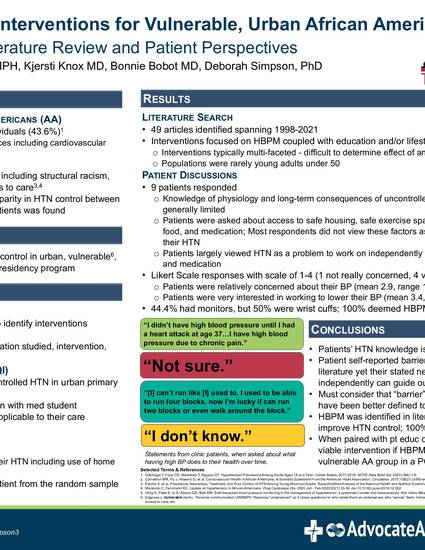
49 articles were identified, spanning 1998-2021, and reviewed. Interventions focused on HBPM coupled with education and/or lifestyle changes. Often interventions were multi-faceted, making it difficult to determine the effect of any single intervention. The populations were rarely young adults under 50.
9 patients were interviewed. Knowledge of physiology and long-term consequence of uncontrolled HTN was generally limited. Barriers for most respondents did not include ability to exercise, access to healthy, affordable food or medications, safety, or housing. Patients largely viewed HTN as a problem they needed to work on independently through diet, exercise, and taking medications. Using a scale of 1-4 (1 not really concerned, 4 very concerned), patients indicated that they were relatively concerned about their blood pressure (mean 2.9, range 1.5-4.0). Using a similar scale, patients were very interested in working to lower their blood pressure (mean 3.4, range 2-4). 44.4% had a blood pressure cuff at home, though 50% owned wrist cuffs. HBPM was seen as viable intervention by 100% of patients.
Conclusions
Patient self-reported barriers were discordant with the literature review findings, providing limited guidance for selecting a clinic-wide HTN intervention. However, HBPM, identified in the literature as a tool to improve HTN control, was of interest to these patients. When paired with patient education on HTN, HBPM may be a viable intervention if blood pressure cuffs were available to this urban, vulnerable African American population in a primary care residency clinic.
Nye R, Lehmann W, Knox K, Bobot B, Simpson D. Identifying hypertension interventions for vulnerable, urban African American primary care patients: Literature review and patient perspectives. Abstract. Alliance of Independent Academic Medical Centers Annual Meeting. New Orleans. March 24-26, 2022
